Verifying Your Patients’ Oral Health for Overall Health Eligibility and Enrollment Status
We’re committed to providing you with the best opportunities to promote the health and wellness of your patients. The additional benefits available to your patients enrolled in our Oral Health for Overall HealthSM program help improve their overall health outcomes.
Services are covered 100% and don’t count toward members’ calendar year maximum. Eliminating out-of-pocket costs increases the likelihood of eligible patients taking advantage of the program’s benefits.
Eligibility, benefit, and periodontal reminders
Your patient is eligible for Oral Health for Overall Health benefits if they:
- Are enrolled in the program
- Have a dental plan that permits enrollment in the program
- Have been diagnosed with an eligible medical condition
- Have any Medicare Advantage plan (except for FHCP)
Patients with BlueDental Prepaid and FHCP dental plans are not eligible.
We recommend that you schedule all four visits during an enrolled member’s first visit.
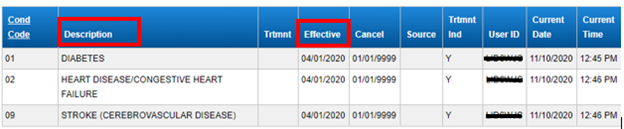
Some of your patients may have eligible conditions and may already be enrolled. If you need assistance identifying patients enrolled in the program, please call 866-445-5148 or log in to the My Patients’ Benefits website and select “Medical Conditions” in the Member Eligibility section. If a patient is enrolled, their conditions and enrollment date are displayed.
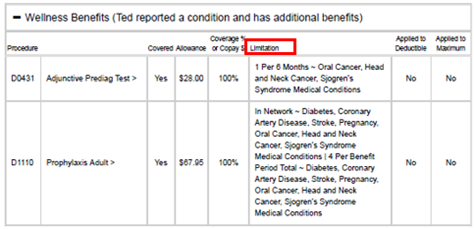
After confirming your enrolled patient’s eligible condition(s), select Benefits and open the “Wellness Benefits” tab. This will display the program benefits details. Details on which procedures/CDTs are covered for which conditions are listed in the “Limitations” column.